Tuberculosis in the context of the COVID-19 pandemic in South Africa
DATE: 8 April 2020
The COVID-19 pandemic reached South Africa in March - the month in which World Tuberculosis (TB) Day is commemorated. The 24th of March is dedicated to reflecting on the impact and advocating for the elimination of TB in individual countries and globally. Dr Sizulu Moyo, research director in the HSRC’s Human and Social Capabilities Programme, discusses TB in the context of COVID-19, highlighting potential areas of concern for South Africa and experiences from the TB response that could benefit and strengthen the country’s response to the pandemic.
TB has affected humans to varying degrees for millennia, with significant implications. In 1993, the World Health Organization (WHO) declared TB a global health emergency. In South Africa, approximately 301 000 people were diagnosed with TB in 2018, and it is the leading natural cause of death in the country. In contrast, the first case of COVID-19 was reported in December 2019, in China, and the disease was declared a pandemic on 11 March 2020. The first case of COVID-19 was reported in South Africa on 5 March 2020, and by 7 April 1,749 people were confirmed positive with the virus and 13 had died from it.
Impact of COVID-19 and TB
Of note is that COVID-19 and pulmonary TB (the most common form of TB) both affect the respiratory system. Therefore, COVID-19 could be more severe in individuals who have TB, given their already existing lung pathology. Furthermore, people who have had TB in the past (TB survivors) may be at greater risk of severe responses to COVID-19, with poorer outcomes, due to residual lung damage from the TB episode. Current knowledge suggests that people with undiagnosed and untreated TB are also at greater risk for severe responses to COVID-19. This risk could be further increased for those living with HIV who have low CD4 cell counts, although there is currently no published data on the co-occurrence of COVID-19 and TB, with or without HIV.

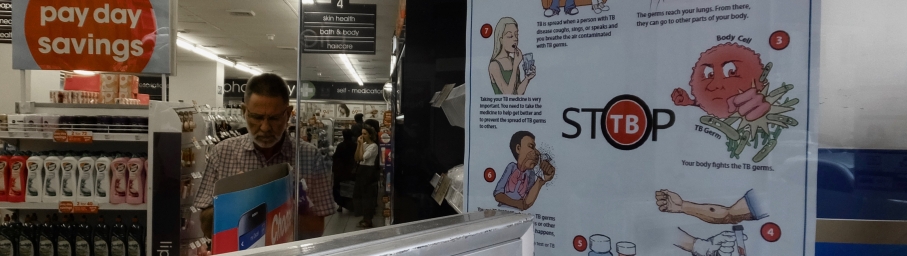
The day before COVID-19 lockdown in South Africa, a poster in a Cape Town pharmacy promoted TB awareness. World Tuberculosis (TB) Day, 24 March, fell in that same week.
Photo: Andrea Teagle
Impact on the health system
Information from China, Europe and North America shows that health systems rapidly become overstretched and barely able to cope with the pandemic, once COVID-19 takes hold. This is a likely scenario for South Africa as the number of local transmissions increase. A strain on the health system would likely arise due to resource diversion to the COVID-19 response for contact tracing, screening, testing and treatment of cases that require hospitalisation. This could delay the diagnosis of those with TB and increase interruption or treatment stoppage among patients already on treatment, with the consequence of reversing the previous gains made towards ending the TB epidemic in the country. The WHO and the STOP TB Partnership have called for efforts to be directed at both conditions. The WHO is also releasing guidelines to help countries maintain essential health services for endemic conditions during the COVID-19 pandemic.
Lessons learned from the TB epidemic
Efforts to fight the TB epidemic in the country provide valuable lessons that can assist the response to COVID-19, including the following:
- Working with Community Healthcare Workers (CHWs): to trace people diagnosed with COVID-19. The TB programme has a well-established system of contact tracing for TB using CHWs, entry-level healthcare workers who work directly with communities. The model of recruiting and training entry-level healthcare workers is already being successfully applied to the COVID-19 response.
- Working with community volunteers and CHWs for raising community awareness and community education: The TB programme works with volunteers who raise awareness about TB in a localised context. This model can be adopted to support the COVID-19 response in different areas across the country.
- Triaging of patients who attend healthcare facilities: Given the high burden of drug-resistant TB, triaging of individuals who might have TB is widely practised in many primary healthcare facilities, which are often the first port of call for people with health problems and will, therefore, likely be the first port of call for many of those who might be infected with COVID-19. Although there is a need for strengthening the triaging process, it will not be a new practice for many healthcare workers in primary health care facilities. Additional measures that are specific to COVID-19 could, therefore, be implemented with minimal training and adaptation in many health care facilities.
- Use of personal protective equipment: The high burden of drug-resistant TB in the country has resulted in many healthcare workers being aware of and trained in the proper use of N95 Respirator masks. TB programme staff can, therefore, be a resource for training other health care workers on the correct fitting and usage of these masks.
- Communication and messaging: TB prevention requires good cough hygiene, including coughing into a flexed elbow or a tissue, among other actions. Appropriate cough hygiene had, therefore, already been communicated widely in South Africa prior to the COVID-19 pandemic. However, anecdotal evidence suggests that individuals have not always adhered to this advice, suggesting a need for continuous and heightened messaging about COVID-19 prevention measures.
- Early adoption of new diagnostic technologies: South Africa was one of the first high TB burden countries to adopt GeneXpert technology for the public sector to expedite the diagnosis of TB. This resulted in early diagnosis and initiation of treatment for many people with TB, and especially those with drug-resistant TB. The country should, therefore, be well prepared for the adoption of validated technologies to aid the COVID-19 response as soon as they are available.
- Dual testing of patients: Given the overlap in symptoms, it will be important to test people with cough and fever for both COVID-19 and TB whenever this is indicated. The South African health system is experienced in implementing testing for TB and HIV co-infection and this experience can be applied to the COVID-19 epidemic in cases where co-infection is a possibility.
Author: Dr Sizulu Moyo, research director in the HSRC’s Human and Social Capabilities Programme
smoyo@hsrc.ac.za